Christian McEachern recalls his time as a peacekeeper in the former Yugoslavia as working “22 or 23 hours a day on the front line, being shot at – or guys are getting killed or wounded with land mines.” During his 14 years in the Canadian Forces, including tours on United Nations-sanctioned peacekeeping missions in the Balkans and Uganda, McEachern witnessed and experienced firsthand a number of horrifying events. “By the time I came home after about a year and a half in Yugoslavia … I was pretty wired,” he says.
Christian McEachern recalls his time as a peacekeeper in the former Yugoslavia as working “22 or 23 hours a day on the front line, being shot at – or guys are getting killed or wounded with land mines.” During his 14 years in the Canadian Forces, including tours on United Nations-sanctioned peacekeeping missions in the Balkans and Uganda, McEachern witnessed and experienced firsthand a number of horrifying events. “By the time I came home after about a year and a half in Yugoslavia … I was pretty wired,” he says. “And it wasn’t just me, it was everybody.”
Upon returning from operations overseas, McEachern and many of his army buddies fell to partying hard. “You could still do your job, but you were making more self-destructive decisions,” he says. “When you look back at my dossier at when I got in trouble at particular times, it was all related to either right after an operation or after a significant event within the military.” Now in his 40s and living outside of Black Diamond, Alberta, McEachern presents the image of a fit, avid outdoorsy-type. He also suffers from post-traumatic stress, and was honourably discharged from the Canadian Forces in 2001.
I first met McEachern in 2009 while conducting research for my PhD in Peace and Conflict Studies at the University of Manitoba. Through conversations with him and other Canadian and American veterans during the past five years, I became aware of a growing grassroots movement among veterans seeking ways beyond conventional treatments to manage their stress injuries. Some are turning to writing groups, meditation and volunteering, but an increasing number are turning to nature – farming and gardening, hiking and fishing, building relationships with dogs or horses. This does not mean conventional treatments are obsolete. Many veterans continue to benefit from medication and therapy, but find that nature provides an additional measure of support, relief and healing in their lives.
After receiving his diagnosis in 1998 and undergoing years of counselling and medication, McEachern describes sitting on the banks of the Columbia River in 2005 and finally feeling “at peace with life for a moment” and realizing “maybe it would be helpful for other veterans to be able to sit here on the river bank, too.” From 2006 to 2011, McEachern ran the non-profit Canadian Veteran Adventure Foundation (CVAF) with a vision to provide another tier of care and treatment for veterans suffering from stress injuries through outdoor programming and adventure training. Among other activities, the CVAF took stress-injured veterans rafting, horseback riding and camping.
Veterans turning to nature for occupation, support and healing has deep roots. In Defiant Gardens, Kenneth Helphand describes how First World War soldiers planted and harvested gardens right in the trenches. “In contrast to war,” he writes, “gardens assert the dignity of life, human and nonhuman, and celebrate it.” Garden therapy was used to treat shell-shocked First World War soldiers, and horticultural therapy was first developed in US veterans’ hospitals during the Second World War.
In 1942, the Canadian government instituted the Veterans’ Land Act, which provided grants, low-interest loans and training for veterans to become farmers, smallholders and commercial fishers. The program supported more than 140,000 veterans before being terminated in 1977.
A 2013 Canadian Department of National Defense (DND) study reports that 13.5 per cent of soldiers who served in Afghanistan from 2001 to 2008 suffer from deployment-related mental injuries. Some experts outside the DND argue the study severely underestimates the number of suffering soldiers and veterans, and suggests the real number could be double. Post-deployment screening reports have found that one in four Canadian soldiers returning from Afghanistan engages in high-risk drinking or experiences negative states ranging from depression to thoughts of suicide.
Invisible injuries have always been part of a soldier’s war experience, and have been described using various terms, including ‘shell shock’ (WWI), ‘battle fatigue’ (WWII), and ‘post-Vietnam syndrome.’ In 1980, post-traumatic stress disorder (PTSD) became the common term to describe combat soldiers’ and veterans’ distress. Today, however, there is growing debate over the term disorder. Many veterans consider their distress to be an appropriate response to the trauma and violence they have experienced and in which they have participated. The umbrella term ‘operational stress injury’ is now used within the Canadian Forces to describe “any persistent psychological difficulty resulting from operational duties performed while serving.” Many veterans favour this term, which emphasizes their suffering as an injury rather than a mental illness.
Symptoms of PTS include nightmares, thought intrusions, physical sensations and flashbacks. It is difficult to predict memory triggers, and because of this many veterans isolate themselves. PTS sufferers can also experience problems falling and/or staying asleep, an inability to concentrate, irritability, intense anger and hypervigilance. Further, many take years to come forward about their suffering for fear of being stigmatized as weak, crazy or fakers.
Humans have long turned to nature to ease what ails us. Most of us have an intuitive sense that walking in the woods, exploring outside with children or working in a garden makes us feel well. There is a growing body of empirical research indicating that nature contact is important for human wellbeing at physical, psychological, cognitive and emotional levels. Theories and research studying the human-nature relationship are diverse, but tend to agree that the human brain evolved in complex environments, in which our survival depended on constant interaction with other creatures and the Earth, and that deep ecological instincts continue to be rooted in the human psyche.
Studies have shown that surgery patients with a view of trees from their hospital beds required a shorter stay and fewer medications and experienced fewer postsurgical complications than patients whose windows looked onto a brick wall. Prison inmates with a view of farm fields used healthcare services less often than those who looked onto an inner courtyard. Other studies have found that blood pressure, anger and aggression all decrease when participants walk at a nature reserve, but increase when participants walk in an urban setting. Children with attention-deficit hyperactivity disorder experience fewer symptoms when they spend time in nature. Elderly nursing home residents who spent time in a garden instead of staying indoors reported both improved moods and lower levels of anxiety, which was confirmed by their significantly lower levels of cortisol, a stress hormone. Physical contact with certain soil bacteria has also been found to have an antidepressant-like effect by boosting serotonin levels.
Neuroscientist Kelly Lambert and her students recently conducted an experiment with rats in which one group received the typical laboratory-enriched environment including plastic toys, tunnels and mirrors, while another group received sticks and leaves, small logs and pebbles. While there was little difference in the rats’ cognitive behaviour, “we are seeing a difference in emotional resilience,” Lambert told me. “The animals in the natural environment are bolder and their stress hormones are at a healthier level.”
Many European countries are putting such research findings into practice by offering ‘green care’ within their wider healthcare programs. For example, in The Netherlands, green care farming (also called social farming) has become a comprehensive, professionalized movement, with more than 1,000 privately owned care farms that earn an income from selling agricultural products, while also offering agriculture-related healthcare activities. A healthcare professional can refer a patient to work on a farm for a continuous period or as a weekly activity – in addition or as an alternative to medication and/or therapy – and farmers are paid to provide this service by healthcare institutions, insurance plans or even directly by clients. Farmers benefit from the added workers, while clients derive health benefits from working on the farm.
Most other European countries offering green care are doing so in a less formal way and catering to a smaller client base. Only Flanders (Belgium), Norway and Slovenia are moving in a similar direction to The Netherlands, with the primary involvement of private farmers. In countries such as Germany and Austria, green care remains the responsibility of healthcare professionals and most care-related gardens and farms are operated by healthcare establishments. In Italy, France and Ireland, volunteer cooperatives provide green care and see it as part of a social philosophy to help clients with mental health difficulties participate in wider society.
The United Kingdom has a growing focus on social and therapeutic horticulture. This movement developed out of traditional horticulture therapy, but celebrates the benefits of social interaction and sense of community in the healing process. Today more than 1,000 programs provide care to more than 21,000 people per week in the UK.
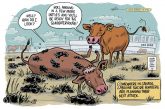
There is no organized discussion of green care in North America. The Canadian government’s 2009 decision to close prison farms suggests an attitude of hostility towards the concept.
However, my research suggests there is a grassroots, veteran-led green care movement in North America. In the US, individuals and organizations such as the Farmer Veteran Coalition (FVC) are finding opportunities for former military personnel to retrain as farmers. The main emphasis of the FVC, which has supported more than 1,000 farmer-veterans in the past six years, is that agriculture provides a viable career option for retired military personnel. “Agriculture is not easy and veterans have a lot of practical skills,” says Tia Christopher, FVC chief of staff and a US Navy veteran. “They also have a huge strength – due to what many of them have lived through – that helps them stick it out in a very, very tough secondary career.”
“In the military, we’re taught to be given a task, to see to that task, and to complete that task. And it’s been hard with prolonged warfare for service members to see the completion of a task … I think there are very negative psychological consequences to that,” Christopher explains. “We’ve found that when veterans can follow a plant cycle, when they prepare the earth, they plant the seed, they nurture it, they harvest it, and they eat it or they sell it – that process in itself is healing.”
My research and conversations with American veterans show that many are gravitating towards small-scale, organic, farms – a trend Tia Christopher confirms. “Even though we have veterans representing all different schools of thought when it comes to agriculture, I’ve found anecdotally that the majority of veterans entering this field want to do sustainable agriculture in some way, shape or form,” she says. “They want it for their own personal health, and then that translates to what they raise for other people, what they want to sell, and how they want to live.” Many veterans also attest to a strong desire to continue serving their communities in meaningful ways, and farming and working outdoors offer possibilities for engaging with plants and animals, nurturing and cultivating new life, and providing healthy foods to feed other people.
Nathan Lewis, an Iraq war veteran, co-founded the non-profit Veterans’ Sanctuary in Ithaca, New York, in 2009. The Veterans’ Sanctuary is a three-fold project that includes a community garden, a writing group and a paper-making initiative, all to support veterans from the wars in Iraq and Afghanistan as they transition to civilian life. “It’s really nice at the end of the day to stop and look at what your labour has produced, to look at something tangible and, without a doubt, positive,” says Lewis about working in the garden.
Lewis suffers from service-related PTS and recalls the period following his return home from Iraq as an “unsteady, dark, troubling time.” He was very unhappy and suffered from extreme anger and deep guilt about his participation in the war. The next few years were filled with heavy drinking, substance abuse and bar fights. This period contrasts sharply with his Veterans’ Sanctuary work. “A lot of vets have trouble sleeping, and I have here and there, but if [I’m] outside with a shovel for eight to 10 hours, and especially doing it as a labour of love, I don’t have trouble sleeping anymore,” he explains. “I want to be out there, so I have no problem whatsoever cranking out a 10 or 12 hour day, and then sleep comes real easy.” He laughs.
The many projects that come with tending a large garden and two greenhouses provide “a lot of anchors into life,” says Lewis. “If you’re feeling bad, and you’re suicidal, you feel very alone and gloomy. Anything that keeps you strapped into this world – into the living – is good. I can’t go nowhere because the beets need watering and the chickens need to be fed. And that’s all I can think to do. I’ve seen too many people go off, fall apart, kill themselves, or just drop out of life, and it’s sad.”
The main goal for the Veterans’ Sanctuary garden is sustainable food security, independence and resilience. “We like to think about and follow a lot of permaculture principles to try to integrate things, instead of just big monocrops,” Lewis explains. “It’s not only food security, but to have real food that is healing and nourishes bodies, so veterans can get their nutrients, and they have a fighting chance to tackle some of the more long-term, deeper spiritual/soul/war trauma issues, to try to sort them out.”
In Canada, veterans’ groups have focused more on outdoor activities. In mid-2011, Christian McEachern’s CVAF disbanded due to a lack of funding. However, he continues to find personal healing through nature, particularly in his relationship with horses. In 2007, he got his first horse, a thoroughbred gelding and ex-racehorse that was having difficulty adjusting to life after racing and was destined for slaughter. The bond and trust that developed was healing for both. Soon after, McEachern rescued a second horse.
“There’s a peace that you can’t really explain when you’re with them,” he says. “You really have to be in the moment with horses. I tend not to think about everything that’s going on when I’m in my zone with them.” McEachern confesses he would not have been in the right frame of mind to accept horses into his life when he first got out of the Forces and was very angry. “That’s not the right place to be when you’re with horses – but I think they came to me at a time when I was ready for them.” He now has six, and when I ask if he rides every day, McEachern replies, “Oh yeah, I try to.”
Working with horses allows veterans to “regain a connection with another social animal in a way that helps build self-confidence, and brings people out of depression.” – Steve Critchley, Canadian Forces veteran & Can Praxis co-founder
Indeed, therapeutic relationships with dogs and horses are a growing area of grassroots veterans’ care in Canada. Several organizations provide specially trained service dogs to veterans and other first responders suffering from stress injuries.
In the spring of 2013, on a ranch northeast of Rocky Mountain House, Alberta, an equine therapy program called Can Praxis began offering its services free of charge to stress-injured Canadian Forces veterans and their spouses. A main benefit of working with horses, says Steve Critchley, Can Praxis co-founder and a 28-year veteran of the Canadian Forces, is that veterans “regain a connection with another social animal in a way that helps build self-confidence, and brings people out of depression.”
Most veterans who participate in Can Praxis gain confidence when they realize a horse will trust them, which then lends to reconnecting with their families. “The horse is a great teacher,” explains Jim Marland, an Equine-Assisted Learning facilitator, psychologist and Can Praxis co-founder. He says a horse will “let you know when something’s not quite right or when it is great. Oftentimes, it’s much easier for [the veterans] to talk about [something] when it’s been pointed out by a horse, [rather] than some psychologist who asks the difficult question.”
Funding is a major challenge for most groups offering nature-based support to veterans. The Outward Bound Canada Veterans Program, which offers weeklong adventure-based resiliency training for Canadian Forces veterans in the Rockies, is one of the few groups that has been successful over a number of years. Project Healing Waters Fly Fishing Canada, which offers fly fishing and fly-tying education and outings to disabled military personnel and veterans, is also expanding its reach throughout Canada.
Unlike in the US, organized opportunities for Canadian veterans to start farming and gardening are almost non-existent, despite the benefits these activities provide. In my conversation with neuroscientist Kelly Lambert, she explained how in the warzone soldiers’ brains help to protect them by making associations with certain sounds and smells. “It was absolutely adaptive and absolutely normal for them to be very vigilant about every little thing in their environment – that kept them alive,” says Lambert. “But the problem is: how do you switch from that vigilance to telling your brain, ‘Ok, I’m in a different environment; I’m safe; I don’t need to be that hypervigilant right now’?”
Lambert believes that nature contact “optimizes the transition from a combat zone.” She says it is important for veterans to help their brains transition to civilian life by weakening some of the associations with sounds, smells and other sensations of the combat zone. “And that’s maybe what they’re doing in some of these farming situations where it is quiet and there aren’t loud noises. They’re not using power tools, they’re using their hands. They’re having some time where they’re not activating those associations.”
It’s time to pay attention to the voices of veterans who are finding paths through suffering and despair by connecting with nature. It’s time to fund and support veteran-led initiatives to make these activities and experiences available to as many veterans as would like to participate – and others, too. It’s time to acknowledge what the research makes clear and what many European countries already know: contact with nature matters. It matters for veterans, it matters for others suffering from injuries and mental health issues, and truly, it matters for all of us.
“There are not many fixes, and gardening’s not a fix, but it’s an effort,” says Iraq war veteran Nathan Lewis. “It gives you a fighting chance. It keeps you in the game. It allows you to take control of your own situation, of your own destiny.”
Contribute by contacting your MP or the Minister of Veterans Affairs and letting them know you support the green care movement and would like to see funding for its therapies and programs. Tell them that post-traumatic stress is often a long-term or even lifetime injury. Use facts from this article. Send them this article.
Stephanie Westlund is the author of Field Exercises: How Veterans Are Healing Themselves through Farming and Outdoor Activities, forthcoming from New Society Publishers in July 2014.